Ring chromosome 20 syndrome [r(20) syndrome] is an ultra-rare, difficult to treat epilepsy, often accompanied by intellectual disability and behaviour disorder. The first notable symptom, seizures, typically presents in early school years following normal childhood development, so chromosome problems are not usually suspected. r(20) syndrome is perceived to be an under-diagnosed and under-reported rare epilepsy and from the evidence our patient group has gathered, the rate of diagnoses is likely in decline. This is a worrying trend and is contradictory to most other rare diseases where giant leaps forward in genetic and genomic understanding are resulting in reductions in the time to diagnosis. So why is this happening and what can we do to reverse this retrograde trend? I’ll try to explain…
Cytogenetic testing is a type of genetic testing that uses samples of tissues to look for anomalies in the Chromosomes. It is most commonly carried out on fetuses of older mothers, screening for newborns and children who have obvious physical differences or developmental delays. Karyotyping is a process in which Chromosomes are observed and ordered and was the first method introduced to look at the shapes and counts of individual Chromosomes, usually from blood samples. This basic technique has since been superseded in favour of more sophisticated technologies that allow for the visualisation of Chromosomes and genetic material in a cell and sequencing of exome and whole genome. This allows more detailed analysis to be performed to identify genetic variants – put simply, scientists can now look for bits of genetic material added, bits duplicated, bits rearranged and bits missing.
These technological advancements represent a step change for the rare disease community as more numerous and more accurate diagnoses are being made every day. But what if for some rare diseases these advancements are resulting in diagnostic decline?
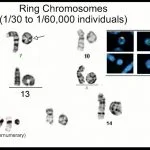
Let’s take ring Chromosomes as an example; in fact, I will specifically reference r(20) syndrome. Ring Chromosomes are not that rare with 1 in 30,000 to 60,000 live births presenting with a ring chromosome. A ring chromosome is formed when the ends of a single chromosome become joined or ‘fuse’ together forming a circular structure (ring), rather than the usual string-like (linear) form.
Why is r(20) syndrome – with chromosome 20 being one of the more common rings – reported to be so ultra-rare with only 200 cases cited in published medical literature worldwide? Could it be the rarity of this biological phenomenon; could it be the dearth of research publications; or are we just not looking hard enough for rings?
I suspect it is a combination, but I will make an argument as to why I suspect the latter scenario is largely behind the low number of diagnoses and should be a cause for concern…

Most individuals with r(20) syndrome are mosaic.
The ring chromosome is only present in a small fraction of the cells in the body, and very low-level mosaicism has been observed in some people with this syndrome.
Genetic testing to identify the cause of epilepsy in an individual includes: epilepsy gene panel testing (which looks for single pathogenic gene implicated for the cause of the epilepsy), CGH array and sometimes exome or whole genome sequencing. None of these tests will identify a ring chromosome, or point to r(20) syndrome – why? Because they don’t report on the physical structure of the chromosome, they report on any unusual changes in its components. Only a minority of people with mosaic r(20) syndrome have a detectable variation (a deletion at the ends of the chromosome) that can be picked-up by these newer tests and further, none of these techniques allow you to ‘see’ the ring formation. Karyotyping allows geneticists to observe the ring shape under the microscope and that is what is needed to make a ring chromosome diagnosis.
So, we have introduced a problem by advancing technology that looks in increasingly smaller detail at the Chromosomes, genes and genome but fails to see the bigger picture – the ring.
What is the answer? We can either go backwards and advocate that clinicians and geneticists revert to karyotyping (unlikely) or we forge forwards and try to see if we can ‘see’ the ring in a different way. That is why Ring20 Research and Support UK are partnering with Illumina launching the programme UNRAVEL: making genomic understanding of r(20) syndrome possible and to educate and raise awareness of the diagnostic odyssey. Our hope is that technologies can be developed to more easily ‘see’ the ring Chromosomes we know exist. If we can achieve that, then not only do we have the potential to increase the diagnostic yield to better understand the phenotypic range of r(20) syndrome, but perhaps we might find some clues as to why the ends of the chromosome stick together and what mechanisms of action are subsequently at work. Who knows what else we might find to help with the diagnosis of other rare conditions?
In my opinion, the ring chromosome is merely a symptom, and we need to identify the root cause of the ring formation if we are to advance research into more effective treatment options in the future.
Ring Chromosomes exist. We need to think outside the box to find them and better understand them. This is a matter of diagnosis. Some clinicians say that achieving a diagnosis is merely a label, especially if it does not directly affect medical treatment; doctors treat symptoms not syndromes. But from the perspective of the patient family this is a blinkered view. Receiving a rare disease diagnosis must be handled sensitively and if information and support in the form of a patient organisation is available to the individual and their family, this can be of great comfort and help with practical day-to-day coping mechanisms, essential for physical, mental and emotional well-being. Patient organisations are great advocates for furthering the research agenda, increasing the number of known individuals enhancing the case for therapeutic research. This is why diagnosis matters.
I suspect ring Chromosomes are not the only genetic anomaly we cannot yet ‘see’ because current focus is on a very small parts of our DNA at a time. In fact, perhaps the so called ‘junk’ DNA does matter more than we think?
Do your bit. Keep an open mind and spread the word.
Accept we do not yet have all the answers; stay curious.
We may continue to strive to find the unknown unknowns, but we should not ignore the unknown knowns (ring Chromosomes) and make these our goal for discovery.
Author: Allison Watson CEO, Ring20 Research and Support UK CIO