Prenatal
Prenatal Diagnosis
- Amniocentesis can diagnose r(20) in the fetus. Usually only found by chance. No genetic counselling provided.
- Risks of anti-seizure medications (ASMs) during pregnancy.
Birth / early years
- Perfectly healthy child – no dysmorphic features. Apparently normal childhood development.
Need: Genetic counselling for prospective parents including reassurance and information about having a child with epilepsy. Females to be advised of risks of taking certain ASMs during pregnancy.
Ideally: Counselling following pre-natal testing.
Family planning advise provided by Epilepsy Specialist nurse.

First & Second symptoms
First symptoms
- Trouble sleeping at night (night terrors). Hyperactive and/or unusual behaviors e.g. running away for no reason. Comprehension problems at school. Auditory processing problems. Tantrums. ADHD or autism suspected. Disbelief of symptoms from HCP’s.
Second symptoms
- Sudden and severe onset of seizures, worse at night with hallucinations. Typically in early school years, sometimes earlier/later Seizures rapidly increasing every day to hourly or more frequently. Cognitive regression. Behaviour disorder.
Need: Parents to be listened to and take their concerns seriously. Appropriate tests to understand cause of apparent ‘hyperactivity’ and other issues. Understand behaviour problems and triggers and how to manage.
Ideally: Referral to tertiary centre (paediatric neurologist) foe complex epilepsy. Video EEG to diagnose seizures, not behavior problems or night terrors. Awareness and recognition of r(20) signs and symptoms.
Treatment
Seizures types
- Predominantly focal (impaired awareness) seizures, absences, tonic clonic seizures. Some patients also present with jerks or drop seizures. Nocturnal seizures present increased SUDEP risk.
Treatment
- Cocktails of anti-seizure medications (ASMs) tried with limited success. VNS therapy, ketogenic diet, rarely steroids or cannabidiols. Some (inappropriate) referrals for brain surgery workup prior to, or even after, confirmed etiology. Emergency meds prescribed.
Need: Understand different seizure types and risk of SUDEP plus mitigating actions. Advice on the likelihood of success with polytherapy. Understand the seriousness and significance of brain surgery.
Ideally: Epilepsy Specialist Nurse to advise on seizure saftey. Counselling for risk of SUDEP. Advice on suitable seizure alert devices. Provision of Care Plan for emergency protocol. Avoid polytherapy with AED’s. Support for KDT implementation.

Diagnosis
diagnosis
- Diagnosis of r(20) typically found by ‘chance’– 2 weeks to 20+ yrs post-epilepsy diagnosis. Not always referred to geneticist – need explanation re mosaicism. No recommended treatment protocol – treatment on a trial and error basis. Patient remains typically refractory to therapies but with range of side effects which can be as debilitating as seizures.
impact on families
- Families devastated on receiving diagnosis as limited information available to them or their medical team. With no prognostic information families are left to wonder what the future holds. Alongside psychological impact, are social isolation and financial impacts to the family, with some parents having to give up paid work to become carers.
Need: Genetic counselling to understand the impact of the diagnosis, prognosis. Balance optimal seizure control vs managing side effects of treatment. Social care suport.
Ideally: Identify cause for epilepsy by running genetic screening and if not identified through epilepsy panel testing or WGS, then run chromosome testing (karyotype) on 50-100 cells to rule out ring Chromosomes prior to epilepsy surgery workup. Provide information on the disease, genetic counselling and referral to patient support group. Explanation about level of mosaicism and what that means n terms of prognosis. Clinical Practice Guidelines or consensus statement available for diagnosis and treatment.
Growing Up
Early school years
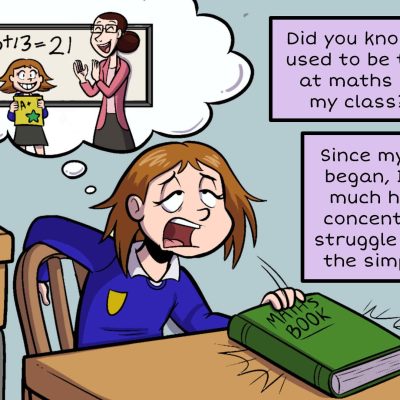
- Frequent seizures impact school attendance, focus, concentration. Teachers do not always recognize seizures/understand learning difficulties.
- Children may lose previously acquired abilities, if seizure control is poor. Wheelchair sometimes required.
- Behaviour and anger/frustration seen typically pre- or post-seizure.
- Seizures more prevalent later in the day (circadian rhythm). Seizures may abate for a period and then return, for no reason
Need: Genetic counselling for prospective parents including reassurance and information about having a child with epilepsy. Females to be advised of risks of taking certain ASMs during pregnancy.
Ideally: Counselling following pre-natal testing.
Family planning advise provided by Epilepsy Specialist nurse.
Adolescence
- Seizures may change in frequency and duration. Longer periods of non-convulsive status epilepticus (NCSE) may be observed. Non-verbally responsive, slowed voice or speak nonsense during a seizure. Still able to carry out activities during a focal seizure.
- Prefer not to be touched during a seizure – liable to thrash out.
- May show autistic traits – prefer routine/OCD – but very social.
- Girls may experience an increase in seizure frequency during menstruation.
- Individuals less socially accepted, fewer friendships than peers. Bullying.
Need: Parents to be listened to and take their concerns seriously. Appropriate tests to understand cause of apparent ‘hyperactivity’ and other issues. Understand behaviour problems and triggers and how to manage.
Ideally: Referral to tertiary centre (paediatric neurologist) foe complex epilepsy. Video EEG to diagnose seizures, not behavior problems or night terrors. Awareness and recognition of r(20) signs and symptoms.

Adulthood
Transition
- Move to adult services is varied – from full transition support to a single handover appointment.
- Fear of changing medications from families – fear of losing level of seizure control.
- Some individuals removed from adult neuro register – nothing more they can do for them.
- Seek independence but require support.
Need: Smooth planned transition into adult services. Reassurance on medication changes. Support in further education and readiness for workplace. Support to access the community safely.
Ideally: Regular (at least annual) follow-up with tertiary centre (neurologist). Consideration of therapeutic history and mutual discussion on changes to treatment.
Adulthood
- Seizures continue and may change over time. Neuro may be unaware of r(20) syndrome – treats seizures rather than syndrome.
- Individuals fear for their future – will their care needs change? No prognosis. Feelings of isolation. Cognitive age may be lower than actual age.
Finding employment can be challenging due to regular seizures and employer’s perception of risk.
Securing financial support remains a battle due to lack of understanding of the disease (as in childhood). Practical support hard to attain. - Risk of passing on r(20) – if inherited child could be non-mosaic (most severe form of r(20)).
Need: Understand prognosis? Lack of research (and no clinical trials in r(20)) means that there is no information on the natural history of the disease, though experience thus far suggests seizures worsen over time. Mental health support. More opportunities for employment with support in the workplace, reasonable adjustments, transport. Help with applications for benefits (as with many living with uncontrolled with epilepsy). Basic needs misunderstood. Support for independent living. Support for parent carers. Eligibility for pratical aids e.g. Support Dogs– need stability in treatment for 6 months. Understand the risks and consequences of having children.
Ideally: Regular blood tests to check for side effects of long-term or changes in ASMs. Appointment of adult social worker to address social care needs. Genetic counselling for those considering parenthood.

Looking for more information?
Download our pdf information sheet on Ring20 or click here for ways to contact us.