I’m not just talking about seizure types, indeed there are over 40 different types of seizure – most people are familiar with tonic clonic seizures (fall to the ground and shake) or absences (brief episodes of staring/blankness), as this is what is more frequently portrayed in the public arena.
Even first aid courses rarely cover the multitude of different types of seizures, so no wonder people experiencing a seizure are misunderstood, maligned or stigmatised in society.
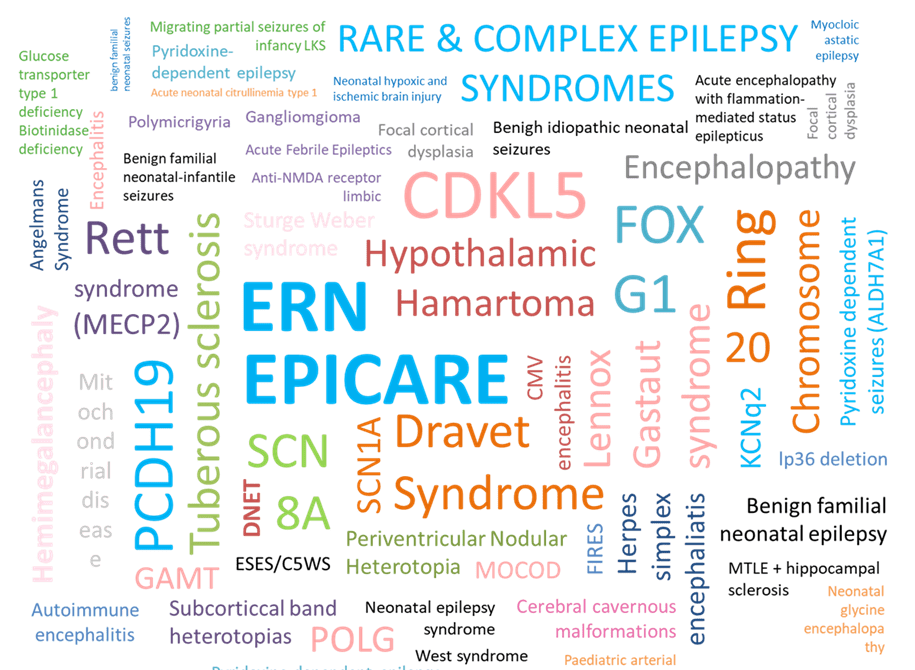
There are over 630,000 people in the UK with epilepsy; 50 million people worldwide – the most common neurological condition we speak so little about. That’s a lot of people, but DID YOU KNOW that epilepsy is not one single condition, but many conditions which can collectively be referred to as:
the epilepsies
Just as there are many different types of cancer, so there are many different types of epilepsy – many of them considered rare diseases in their own right.
I imagine you can name several types of cancer, but how many of the epilepsies can you name?
Seizures (bursts of abnormal electrical activity in the brain) are often only one part of someone’s epilepsy (recurrent seizures). A person living with epilepsy may also experience other symptoms and these may vary dependent on the cause of the epilepsy. Intellectual impairment and behaviour disorders are some of the most commonly reported co-occurring symptoms in people whose epilepsy is difficult to control – so called drug-resistant epilepsy (DRE) – there are many other possible symptoms (comorbidities), too many to name here. We’re not always sure if these are separate to, or a consequence of, the epilepsy itself.

1 in 3 people live with uncontrolled seizures

Why does it matter that we understand the cause (aetiology) of someone’s epilepsy and other symptoms? Aren’t we just adding another label? Well, no, there are direct and indirect benefits from more specific diagnoses – from more targeted treatment options, to information and support. For example, someone with a structural change in their brain e.g. a brain tumour, may be assessed for eligibility for brain surgery (which could even result in a cure), whereas someone with a genetic variation may respond more favourably to specific medications or alternative treatment such as ketogenic diet, or possible gene therapy. Some epilepsies are caused by head injuries or serious illnesses that affect the brain. The list goes on…
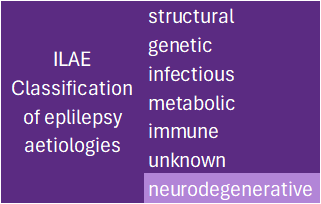
Classifying epilepsies helps to group them. Note: these classifications are not mutually exclusive – a person can have more than one classification for their epilepsy – it can get complicated!
Not all diagnoses for the epilepsies are arrived at via a definitive test, a good example being Lennox Gastaut Syndrome (LGS) which is given as a ‘clinical diagnosis’ when a person displays a predefined collection of symptoms. But this collection of symptoms can be subjective, open to different interpretations by different doctors in different countries and has changed over time – so someone who received their diagnosis 20 or more years ago may/may not fit the criteria for a clinical diagnosis today. With improved diagnostics we can now potentially identify the underlying cause for someone’s LGS, so the LGS becomes a secondary diagnosis. And this is significant because…as previously stated a diagnosis for your epilepsy can influence treatment options, access to research or clinical trials which could change your life. Or not, as a more specific diagnosis that would previously have been categorised clinically as LGS, may preclude access – so we have a double-edged sword.
We are entering a new phase of discovery with the advent of the Epilepsy Research Institute and recent additional UK government funding for research which brings hope for the future. With the diversity of the epilepsies there is a huge mountain to navigate but we will never find the answers if we don’t try. We are now seeing advances towards so called ‘precision medicine’ with emerging gene therapies for some epilepsies.
I hope you can see that with many different underlying causes for epilepsy, we need many different therapeutic approaches.
Advancing scientific discovery into the underlying causes of the epilepsies
will help us to find better treatments in the future.
Most epilepsies start either in childhood or in older age. A group of the epilepsies are referred to as childhood epilepsies, which can be misleading, suggesting they only exist within children. The most difficult to treat seizures may start in children before the age of 5 years old (sometimes later) and often are found to have a genetic origin, yet many of those children grow up into adults. Some children grow out of their epilepsy, but this depends on the cause so should never be assumed – another reason for more accurate diagnoses. Older adults with currently no known cause (idiopathic) for their epilepsy whose seizures started in childhood, may not have undergone the most advanced tests and investigations that are available today – be that more detailed MRI, improved EEG, or genetic/genomic testing. How many adults affected could reap the benefits of a more accurate diagnosis and may actually have a so-called ‘childhood epilepsy’? Importantly what could we learn from the older generations about the progress of these diseases over time (natural history)? Families with children diagnosed with a rare and complex epilepsy who have transitioned to adult neurological services say how they feel like they ‘fall off a cliff edge’ and that the underlying cause for the epilepsy seems no longer relevant to their medical team or the person’s ongoing care and treatment – which is disappointing. We need to reframe ‘childhood onset epilepsies’ and what they mean in later life.
Unfortunately, there are still too many people whose seizures remain difficult to treat. Uncontrolled seizures are not only life-changing but can be life-limiting.
It’s common knowledge that some cancers can kill, but why do we not speak more openly about the epilepsies in this way?
There are 3 epilepsy related deaths every day in the UK from seizure related causes
Patient support groups, such as Ring20 Research and Support exist to connect individuals and families for mutual, practical support, where medicine doesn’t have the answers YET…collectively as founders of the UK Rare Epilepsies Together (UKRET) network we aim to improve access to diagnosis, treatment, and care in the UK for all the rare epilepsies.
If you have epilepsy, did you know about ‘the epilepsies’? Has this made you curious to find out more? And if you don’t have or know someone who has epilepsy, has this changed your perception in any way?
This Purple Day let’s celebrate the epilepsies together.
To find out more about the signs and symptoms of Ring Chromosome 20 Syndrome click here.
Author: Allison Watson, CEO Ring20 Research and Support UK CIO
March 2024

Statistical references taken from the Epilepsy Research Institute and Epilepsy Action.